As sexually transmitted diseases continue to spread in 2025, a new vaccine candidate may reduce the number of chlamydia cases in the United States. Current programs to prevent infection rates from rising have proven insufficient, highlighting the urgent public health need for a vaccine.
Sanofi announced today that the U.S. Food and Drug Administration has granted a fast-track designation to Sanofi's mRNA vaccine candidate for preventing chlamydia infection.
The chlamydia vaccine candidate has been designed to protect against primary genital tract infection and reinfection by the bacterium Chlamydia trachomatis.
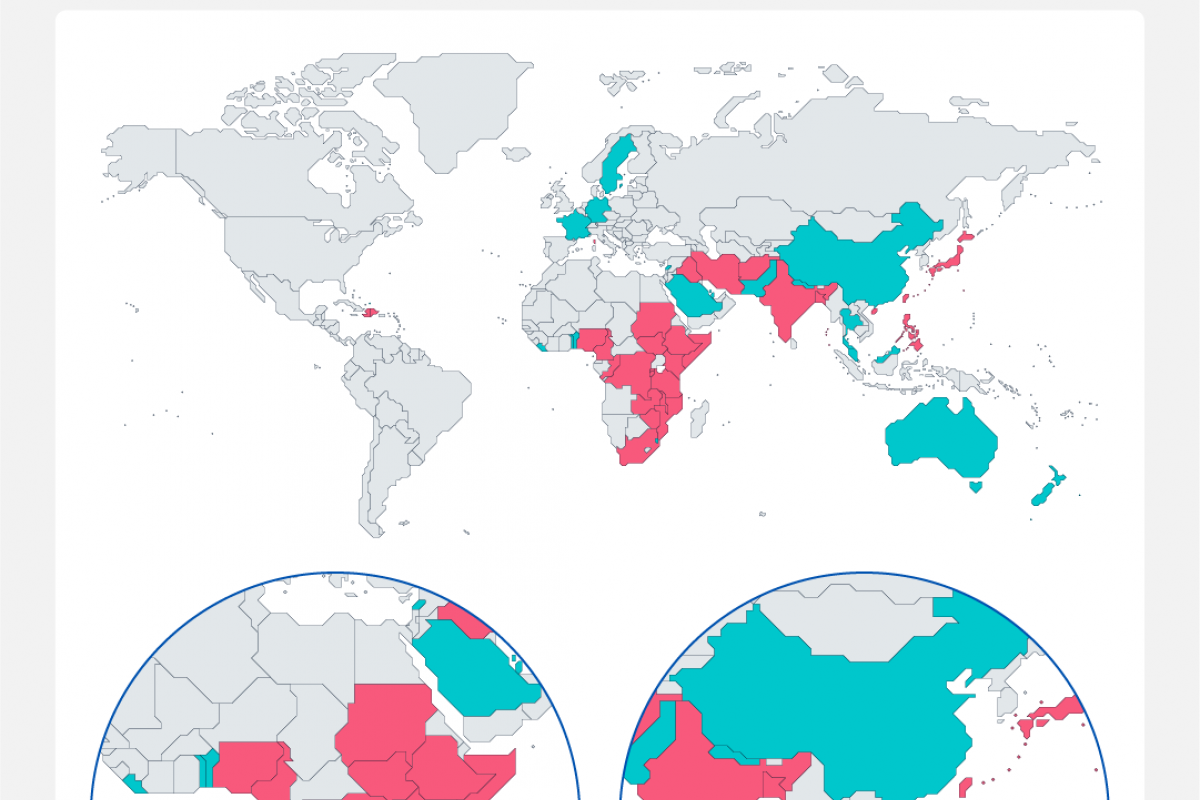
In 2020, there were 129 million worldwide cases of chlamydia among adults and adolescents, with the highest rates of infection among younger people.
Jean-François Toussaint, Global Head of Vaccines R&D, stated in a press release on March 26, 2025, "Millions of people currently live with undiagnosed chlamydia, including asymptomatic infection that can also cause severe long-term health effects if left untreated."
"Antibiotics to treat chlamydia have not been successful in controlling rising infection rates. With our program, we aim to make chlamydia a preventable disease through vaccination."
Following a promising preclinical program, Sanofi is planning a phase 1/2 randomized clinical study to evaluate the immunogenicity and safety of the chlamydia vaccine candidate in adults aged 18 to 29.
This clinical study is due to start in the coming days.
Chlamydia, caused by the bacterium Chlamydia trachomatis, is a common bacterial infection of the reproductive tract with consequences for developing infertility and pregnancy complications.
Although chlamydia can be treated with antibiotics when diagnosed, over 80% of chlamydia cases are asymptomatic, meaning there is a significant risk that infections go unrecognized, leading to untreated cases and unintentional transmission.
A study published by the Annals of Family Medicine on March 24, 2025, indicates that many women are not receiving guideline-adherent treatment in primary care settings. For example, the time to treat chlamydia was longer for patients aged 50-59 years (time ratio relative to those aged 20-29 years = 1.61; 95% CI, 1.12-2.30).
The development of this vaccine candidate is part of the Translational Science Hub, a partnership with the Queensland Government, Griffith University, and the University of Queensland that connects world-class researchers in Queensland, Australia, with Sanofi scientists in France and the U.S.
As of late March 2025, the FDA, the United Kingdom, and the European Medicines Agency have not approved a vaccine to prevent chlamydia infections.