Indonesia's Polio Outbreak Becomes an International Concern

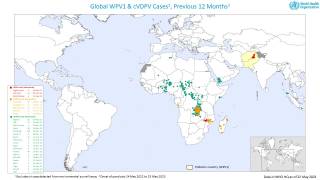
Indonesia's Ministry of Health notified World Health Organization (WHO) in November 2022 of a confirmed case of circulating vaccine-derived poliovirus type 2 (cVDPV2) with acute flaccid paralysis (AFP) from Pidie district in Aceh province.
There is low population immunity against all polioviruses in Indonesia but primarily type 2 in children born after the switch from the trivalent to the bivalent Oral Polio Vaccine (bOPV) in April 2016.
In response to this notification, Indonesia launched an immunization campaign for children under the age of 13 years in the affected areas on November 28, 2022.
The WHO announced on December 19, 2022, that it assesses the risk to be high at the national level due to low polio vaccination coverage in Aceh and other provinces in Indonesia.
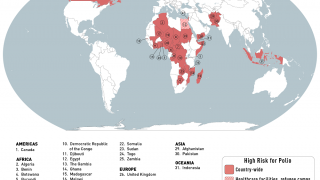
Furthermore, the WHO's current international travel recommendations say that all travelers to polio-affected areas be fully vaccinated against polio.
Before the recent pandemic, millions of people visited Indonesia annually.
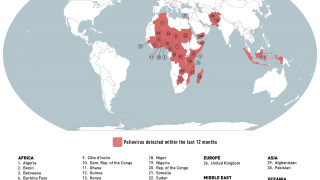
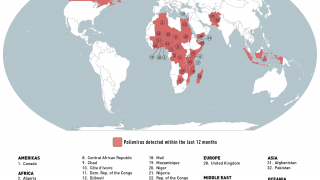
Previously, the U.S. Centers for Disease Control and Prevention (CDC) issued an Alert - Level 2, Practice Enhanced Precautions on November 30, 2022, increasing awareness of polio outbreaks in various countries, such as countries in Africa, Asia, Europe, India, Israel, and the United Kingdom.
The state of New York has been reporting the detection of poliovirus in wastewater samples (94) since April 2022.
The CDC also announced on November 30, 2022, that it would expand wastewater testing for poliovirus in select jurisdictions across the country outside of New York.
It is essential that all countries, particularly those with frequent travel and contacts with polio-affected countries and areas, strengthen surveillance for AFP cases and commence any planned expansion of environmental surveillance to rapidly detect any new virus importation and facilitate a rapid response, says the WHO.
Polio is a highly infectious disease that primarily affects children under five years of age, causing permanent paralysis (approximately 1 in 200 infections) or death (2-10% of those paralyzed).
The virus is transmitted by person-to-person, mainly through the fecal-oral route or, less frequently, by a common vehicle (e.g., contaminated water or food) and multiplies in the intestine, from where it can invade the nervous system and cause paralysis.
Up to 90% of those infected are either asymptomatic or experience mild symptoms, and the disease usually goes unrecognized.
Vaccine-derived poliovirus is a well-documented strain of poliovirus mutated from the strain contained initially in OPV.
In rare instances, the vaccine-derived virus can genetically change into a form that can cause paralysis, as does the wild poliovirus.
This is what is known as a vaccine-derived poliovirus (VDPV).
The detection of VDPV in at least two different sources and at least two months apart that are genetically linked, showing evidence of transmission in the community, should be classified as 'circulating' vaccine-derived poliovirus type 2 (cVDPV2).
Circulating vaccine-derived poliovirus type 2 continues to affect different areas of the world, says the WHO.
Other polio outbreak news is posted at PrecisionVaccinations.com/Polio.
Our Trust Standards: Medical Advisory Committee