HPV Vaccine Knocking-Out Cervical Cancer in Australia

Australian women have been fortunate to have had a government-sponsored cervical cancer vaccine program since 2007.
And 8 years later, the results are very positive.
Cervical cancer death rates in Australia have halved since the National Cervical Screening Program began in 1991. In 2015, there were 230 deaths caused by cervical cancer in Australia.
A new, multi-year study in Australia has shown that this Human papillomavirus (HPV) vaccination program has virtually eliminated new virus infections responsible for cervical cancer for girls who were immunized when they were young teenagers.
** Schedule Vaccine Appointments Here **
Even those who were not vaccinated benefited from the ‘herd immunity.’
This study shows the prevalence of vaccine-targeted HPV types continued to decline among young women.
Moreover, a substantial decrease also occurred in women aged 25–35, despite lower vaccine coverage.
This study reviewed a quadrivalent HPV vaccination program targeting females aged 12–13 years, with catch-up vaccination of 14 to 26-year-olds through 2009. And evaluated the program’s impact on HPV prevalence among women aged 18–35 in 2015.
For the 2015 review, the 3-dose vaccine coverage was 53.3 percent, which means a large number of women had not completed the prescribed therapy.
The results showed the prevalence of HPV types decreased from 22.7% (2005–2007) and 7.3% (2010–2012) to just 1.5% (2015) among women aged 18–24.
And, from 11.8% (2005–2007) to 1.1% (2015) among those aged 25–35.
Human papillomavirus vaccines have undoubtedly exceeded expectations in preventing oncogenic HPV infection, the underlying precipitant of cervical cancer.
Both the bivalent HPV vaccine and quadrivalent HPV vaccines induce high-level antibody responses to HPV16 and 18, which are responsible for 71 percent of cervical cancer cases globally.
This new Australian study’s results were very similar to a recent six-year follow-up study of Dutch women. This study reported nearly full protection against vaccine-type persistent infections and significant cross-protection to non-vaccine types in a population-based cohort.
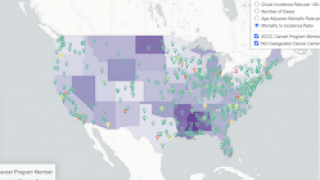
Cervical cancer is associated with several serotypes of the human papillomavirus and is fourth most frequent cancer in women, says the World Health Organization (WHO).
Cervical cancer is the growth of abnormal cells in the lining of the cervix. The most common cervical cancer is squamous cell carcinoma, accounting for 80% of cases, says the WHO.
In the USA, 2 prophylactic HPV vaccines are licensed and each vaccine confers protection against HPV types 16 and 18: Gardasil, Gardasil-9.
These HPV vaccines can be found in most pharmacies in the USA. The CDC Vaccine Price List provides HPV vaccine prices for general information.
And vaccine discounts can be found here.
Vaccines, like any medicine, can have side effects, says the CDC. You are encouraged to report negative side effects of vaccines to the FDA or CDC.
Our Trust Standards: Medical Advisory Committee
- Very Low Prevalence of Vaccine Human Papillomavirus Types Among 18- to 35-Year Old Australian Women
- High Effectiveness of the Bivalent Human Papillomavirus (HPV) Vaccine Against Incident and Persistent HPV Infections
- Prevalence and Incidence of Anal and Cervical High-Risk Human Papillomavirus (HPV) Types Covered by Current HPV Vaccines
- Cervical cancer
- HPV Vaccination Rates in Males Increased Over 200%