Melanoma’s Return Delayed by Personalized Cancer Vaccine
A Texas-based biopharmaceutical company presented the primary analysis of the Phase IIb clinical trial evaluating its tumor lysate, particle-loaded, dendritic cell (TLPLDC) vaccine, in patients with Stage III and IV resected melanoma.
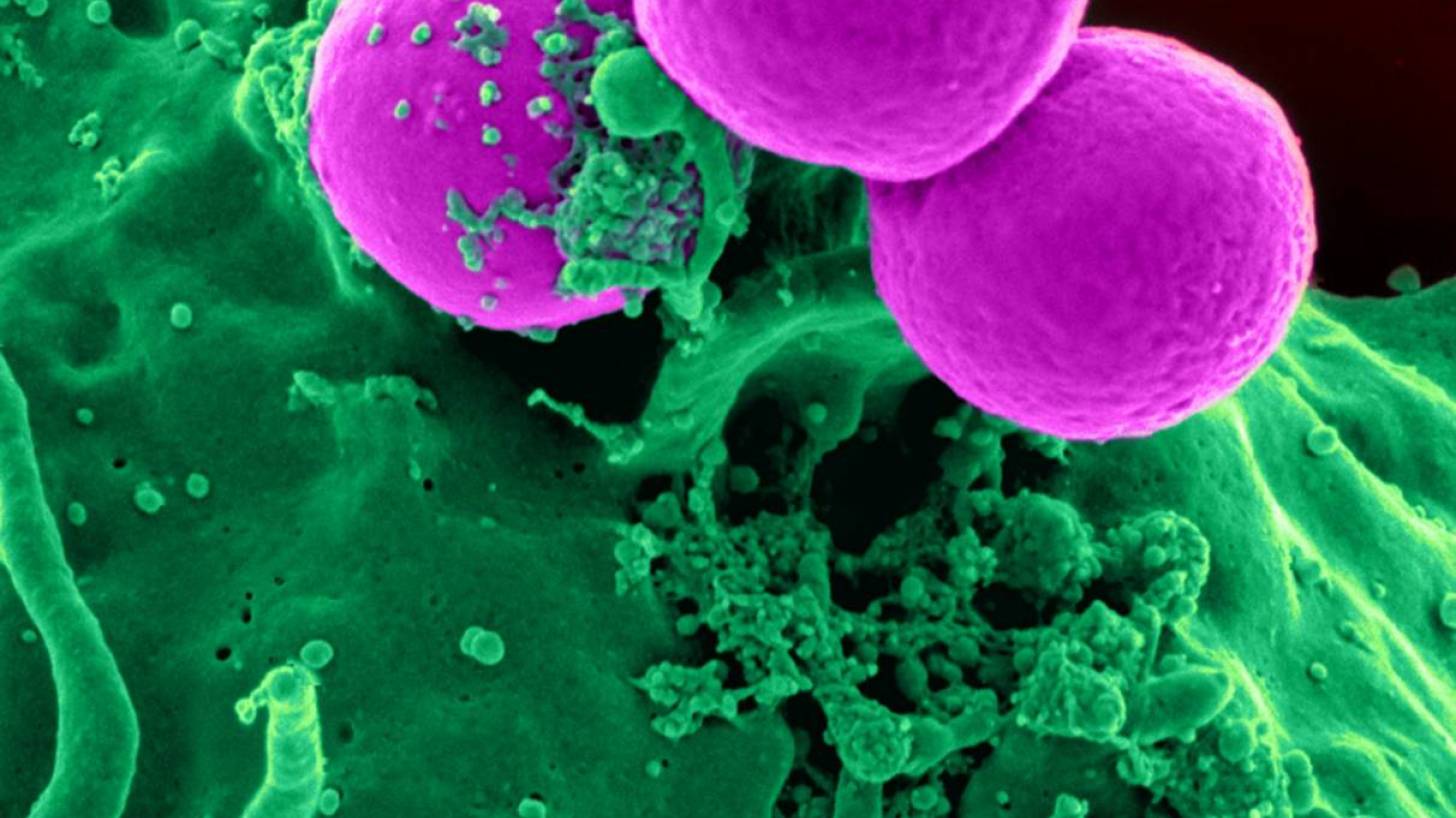
TLPLDC is an autologous therapeutic cancer vaccine that is made from a patient’s own cells and is designed to stimulate the immune system to recognize tumor cells and fight the patient's specific cancer.
Elios Therapeutics announced on November 22, 2019, the initial assessment of 36-month follow-up data on all patients in this study indicated that the ‘TLPLDC vaccine benefit is not only durable but continues to increase beyond 24-months.’
The full study results are anticipated in June 2020.
"Therapeutic cancer vaccines are an attractive alternative immunotherapy because of their potential safety, specificity, and long-lasting response due to stimulation of immune memory," said Mark B. Faries, M.D., co-director of the Melanoma Program and head of Surgical Oncology at The Angeles Clinic and Research Institute, an affiliate of Cedars-Sinai, in a press release.
In the study, 144 participants were randomized to receive either the vaccine or placebo to prevent a recurrence. The vaccines were initiated within three months of completion of standard of care therapy at 0, 1, 2, 6, 12, and 18 months.
The primary endpoint was 24-month disease-free survival (DFS). The pre-specified per treatment (PT) analysis included all patients who completed the primary TLPLDC or placebo vaccine series (PVS) at six months.
In the PT analysis, 24-month DFS was significantly improved in the TLPLDC vaccine group compared to placebo [62.9% vs. 34.8%; (HR=0.52, 95% CI: 0.27-0.98, p<0.041)], representing a nearly 60% reduction in the relative risk of disease recurrence.
There was a non-significant improvement in 24-month DFS between the TLPLDC and placebo arms in the intent-to-treat (ITT) analysis [38.5% versus 27%, (p=0.974)], but a stronger trend in improved 24-month overall survival (OS) in this analysis [86.4% vs. 75.1% (p=0.15)].
Therapy was well-tolerated with 31.7% of placebo patients and 35.9% of TLPLDC patients experiencing a related adverse event, the majority of which were grade 1 or 2.
Samples are collected at resection, frozen, and sent to the lab where they are used to create autologous tumor lysate, which is loaded into yeast cell wall particles (YCWP). This combination is then introduced to the patient's dendritic cells, leading to the creation of the final TLPLDC vaccine.
The time from resection to injection of the vaccine takes approximately 3 weeks.
"This is a very different and personalized approach that is able to deliver each patient's unique composite of tumor antigens to the immune system," said John R. Hyngstrom, M.D., surgical oncologist at the Huntsman Cancer Institute and associate professor of surgery at the University of Utah.
"Administered in a 6-month regimen, the vaccine ignites an innate and adaptive response that trains a patient's immune system to 'see' melanoma cells and any of the specific proteins from their tumor that may be circulating throughout the body and kill them.”
“A vaccine that can provide a protective benefit against melanoma would represent an important new tool for patients and their physicians," he added.
Skin cancer is the most common of all cancers. However, melanoma accounts for only about 1 percent of skin cancers, but causes a large majority of skin cancer deaths, says Cancer.org.
Melanoma is more likely to grow and spread than other types of skin cancer.
When diagnosed and treated at an early stage, melanoma has a high cure rate, however, patients with later stages of the disease carry a high risk for melanoma recurrence because some melanoma cells can remain in the body, even after surgery.
In the U.S, the incidence of melanoma has increased over the past decades, with 91,270 estimated new cases and 9,320 related deaths in 2018, reports Cancer.org.
The TLPLDC (tumor lysate, particle-loaded, dendritic cell) vaccine is a unique type of immunotherapy, both in how it is made and how it is delivered.
Every patient's tumor has a unique antigenic profile unlike any other, and dendritic cells found in the blood are the most potent antigen-presenting cells in the body.
Once TLPLDC is administered, it delivers the patient's complete repertoire of tumor antigens to the immune system, creating a dual innate and adaptive immune response, activating fighter T cells, and triggering the immune system to recognize, and seek out and destroy any cells containing the antigens and specific mutations from their tumor.
Elios has simplified the process so the time from resection to injection is approximately 2 weeks.
This makes the TLPLDC vaccine highly feasible and will ultimately be easy for community and academic oncologists to adopt into their practices.
The TLPLDC vaccine is currently being studied as a monotherapy and in combination with standard-of-care checkpoint inhibitor therapies in a Phase IIb clinical trial for the treatment of late-stage melanoma at leading academic cancer centers in the United States.
Elios Therapeutics, LLC, is a biopharmaceutical company developing a portfolio of innovative personalized therapeutic cancer vaccines targeting unmet medical needs across a broad range of tumor types. For more information, please visit Elios Therapeutics.
Melanoma news published by Vax-Before-Cancer
Our Trust Standards: Medical Advisory Committee