Hepatitis A Outbreak Reaches 10,582 Cases During 2018

The liver disease, hepatitis A had a very good year during 2018, increasing the total number of confirmed cases by approximately 300 percent in just one year.
According to new data from the Centers for Disease Control and Prevention (CDC), as of December 15, 2018, there were 10,582 confirmed hepatitis A cases in the USA.
This increase was ‘bad-news’ for 3 groups of Americans; international travelers, food service staff and those living in Heartland states.
This hepatitis A outbreak began in Michigan in 2016, says the CDC.
The Detroit Free Press reported Michigan led the nation in hepatitis cases per capita during 2017.
Previously, hepatitis A rates in the USA declined by more than 95 percent after the vaccine became available in 1995.
Between 2015 and 2016, hepatitis A cases again increased by 44 percent, from 1,390 in 2015 to 2,007 cases in 2016. After adjusting for under-reporting, the estimated number of new HAV infections in 2016 was 4,000.
During 2017, there were only 3,164 hepatitis A cases reported by 15 states.
During 2018, several ‘heartland’ states reported hepatitis A cases by restaurant staff.
Hepatitis A virus (HAV) is a communicable disease of the liver caused by the hepatitis A virus and is a nonenveloped RNA virus, classified as a picornavirus.
Hepatitis A, hepatitis B, and hepatitis C are liver infections caused by 3 different viruses, which can affect the liver differently.
HAV cannot be differentiated from other types of viral hepatitis on the basis of clinical or epidemiologic features. Diagnosis requires a positive test for antibody to HAV (anti-HAV) IgM in serum, which is detectable from 2 weeks before the onset of symptoms to approximately 6 months afterward.
HAV is usually transmitted by consumption of contaminated food or water, says the CDC.
In the USA, the most frequently identified risk factors for hepatitis A are international travel, person-to-person through the fecal-oral route and exposure to contaminated food or water, says the CDC.
Travel-related hepatitis A can occur in travelers who visit developing countries with “standard” tourist itineraries, accommodations and eating behaviors.
The risk is highest for those who live in or visit rural areas, hike in backcountry areas, or frequently eat or drink in settings of poor sanitation.
According to the CDC, the safety of hepatitis A vaccine for pregnant women has not yet been determined.
A recent review of the Vaccine Adverse Event Reporting System did not identify any concerning patterns of adverse events in pregnant women or their infants after hepatitis A vaccination.
Moreover, international travelers who are exposed to HAV and who have not received hepatitis A vaccine previously should be administered 1 dose of monovalent hepatitis A vaccine or IG as soon as possible.
On November 2, 2018, the CDC’s Advisory Committee on Immunization Practices (ACIP) committee’s updated travel vaccination suggestions.
The CDC publishes a list of countries where hepatitis A is a high-risk at this webpage.
The best prevention from a hepatitis A infection is from vaccination.
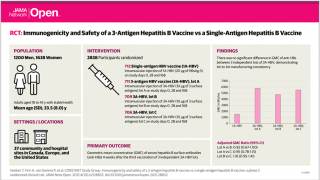
Two monovalent hepatitis A vaccines, Vaqta and Havrix, are approved for people older than 1 year of age in a 2-dose series, and a combined hepatitis A and hepatitis B vaccine, Twinrix, is approved for people older than 18 years of age in the USA.
The immunogenicity of the combination vaccine is equivalent to that of the monovalent hepatitis A and hepatitis B vaccines says the CDC.
To request a travel vaccination counseling appointment at a local pharmacy, please visit this page.
The CDC Vaccine Price List displays current hepatitis vaccine contract prices and general information.
And, hepatitis vaccine discounts can be found here.
Vaccines, like any medicine, can have side effects. You are encouraged to report negative side effects of vaccines to the FDA or CDC.
Our Trust Standards: Medical Advisory Committee