Tennessee Joins Hepatitis A Outbreak in America’s Heartland

The state of Tennessee issued a health alert on May 25, 2018, for Nashville residents to be aware of an ongoing hepatitis A outbreak.
Tennessee now joins America’s Heartland states of Arkansas, Indiana, Kentucky, Michigan, Ohio, and West Virginia in combating this multi-state, multi-year hepatitis A epidemic.
According to reporting by The Tennessean, 14 people from the Nashville area have contracted hepatitis A over the past 6 months.
To reduce this Nashville outbreak, the Metro Public Health Department is offering free vaccinations beginning June 5, 2018.
But, vaccine supply may become a constraint.
The Nashville health department currently has only about 1,150 hepatitis A vaccine doses, according to an agency email obtained by The Tennessean.
Neighborhood Health, a clinic network that will help give out the Metro Health vaccines, said the current supply will cover "less than 5 percent of the at-risk population."
“Neighborhood Health alone knows there are over 18,000 (gay and bisexual men). And we have an unknown number of drug users,” said Brian Haile, Neighborhood Health CEO.
Although this hepatitis A outbreak was not announced to the public until May 25th, Dr. Bill Paul, the Nashville Metro Health director, sent a mass email Thursday, urging a coordinated response.
'We anticipate that this outbreak will get bigger and require a vigorous response over many months by many organizations,” Paul wrote in his email.
Dr. Paul added that Metro Health will prioritize vaccination of drug users and gay and bisexual men because 12 of the 14 known cases appear to be connected with these groups.
Food-related outbreaks of Hepatitis A are often associated with contamination of food during preparation, by the highly contagious person.
Since March 2017, the Centers for Disease Control and Prevention (CDC) Division of Viral Hepatitis has been assisting several states with hepatitis A outbreaks, spread through person to person contact.
The CDC says most adults with hepatitis A have symptoms, including fatigue, low appetite, stomach pain, nausea, and jaundice, that usually resolve within 2 months of infection.
During 2018, the CDC has issued hepatitis A alerts:
“Some of the at-risk Hepatitis A groups include international travelers, persons with chronic liver disease or a clotting-factor disorder,” said Natasha Gildersleeve, PharmD, MTM Clinical Pharmacist at Brookshire Grocery Company.
“Ask your doctor or your pharmacist if you need to be vaccinated against Hepatitis A," said Gildersleeve.
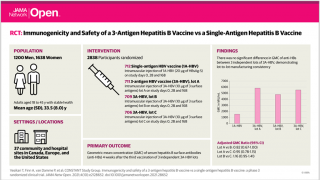
In the USA, there are three FDA-approved hepatitis A vaccines: Vaqta, Havrix, and Twinrix.
Most pharmacies offer these hepatitis vaccines. To schedule a vaccination appointment, please click here.
The CDC Vaccine Price List provides current HAV vaccine contract prices and general information, and vaccine discounts can be found here.
For people who do have contact with a person with Hepatitis A virus, Post Exposure Prophylaxis (PEP) is recommended by the CDC for unvaccinated people who have been exposed during the previous 2 weeks.
People with evidence of previous vaccination do not require PEP.
PEP consists of:
- Hepatitis A vaccine for people aged 1-40 years
- Hepatitis A virus-specific immunoglobulin (IG) for people outside of this age range. If immunoglobulin is not available, hepatitis A vaccine can be substituted.
Vaccines, like any medicine, can have side effects, says the CDC. You are encouraged to report negative side effects of vaccines to the FDA or CDC.
Our Trust Standards: Medical Advisory Committee