It Ain’t Over Till It’s Over…but It’s Never Over
"As I prepare to step down from my dual positions at the National Institute of Allergy and Infectious Diseases (NIAID), where I have been a physician-scientist for 54 years and the director for 38 years, a bit of reflection is inevitable," wrote Anthony S. Fauci, M.D.
"As I think back over my career, what stands out most is the striking evolution of the field of infectious diseases and the changing perception of the importance and relevance of the field by both the academic community and the public," continued Dr. Fauci in a Perspective published by the New England Journal of Medicine on November 26, 2022.
Excerpts from this Perspective are edited and inserted below:
In the 1960s and 1970s, most physicians were aware of the possibility of pandemics, in light of the familiar precedent of the historic influenza pandemic of 1918, as well as the more recent influenza pandemics of 1957 and 1968.
However, the emergence of a truly new infectious disease that could dramatically affect society was still a purely hypothetical concept.
That all changed in the summer of 1981 with the recognition of the first cases of what would become known as AIDS.
The global impact of this disease is staggering: since the pandemic's start, more than 84 million people have been infected with HIV, the virus that causes AIDS, of whom 40 million have died.
In 2021 alone, 650,000 people died from AIDS-related conditions, and 1.5 million were newly infected.
Today, more than 38 million people are living with HIV.
Although a safe and effective HIV vaccine has not yet been developed, scientific advances led to the development of highly effective antiretroviral drugs that have transformed HIV infection from an almost-always-fatal disease to a manageable chronic disease associated with a nearly normal life expectancy.
HIV/AIDS continues, exacting a terrible toll in morbidity and mortality 41 years after it was first recognized.
If there is any silver lining to the emergence of HIV/AIDS.
It is that the disease sharply increased interest in infectious diseases among young people entering the field of medicine.
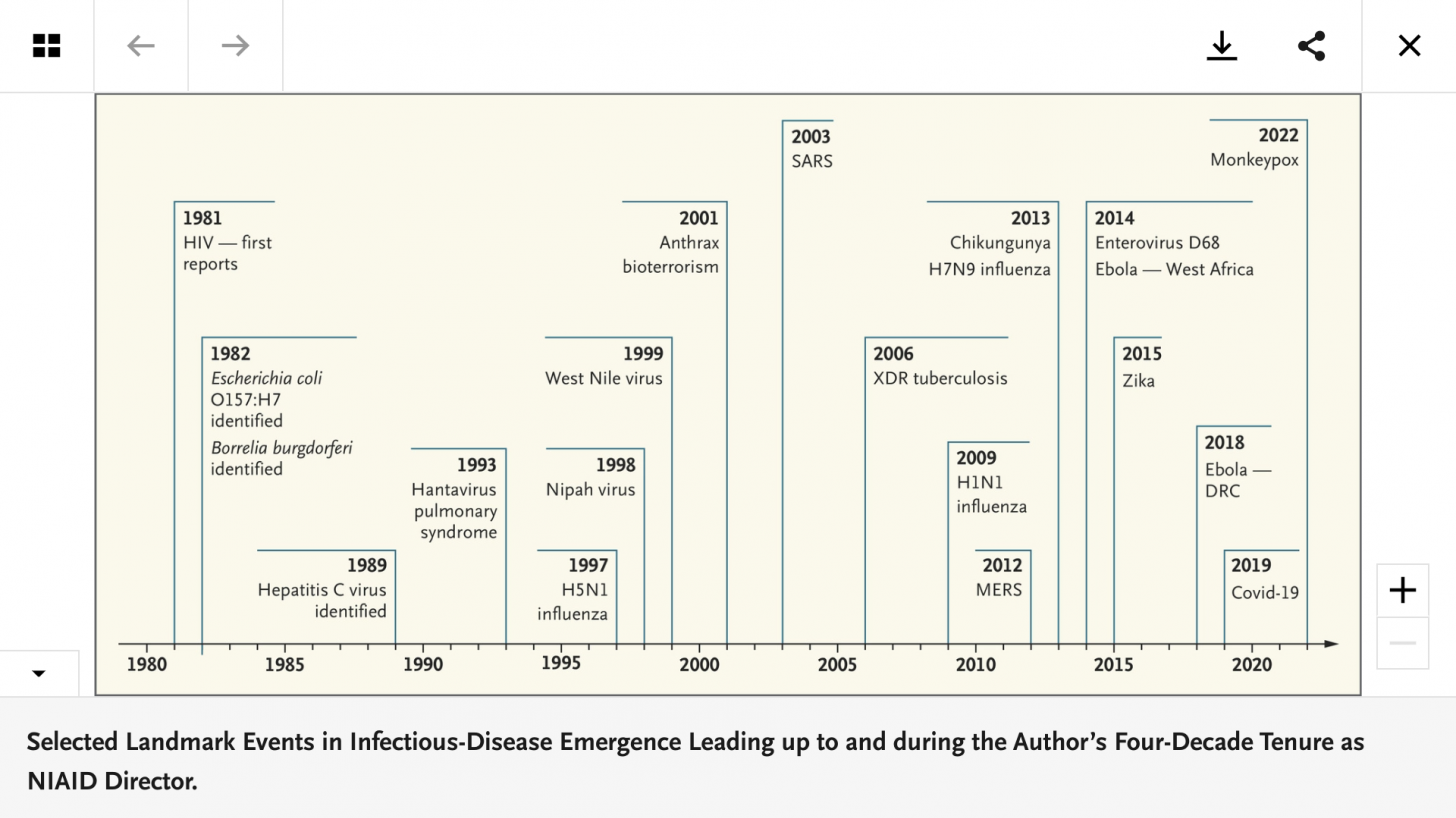
Of course, the threat and reality of emerging infections did not stop with HIV/AIDS.
During my tenure as NIAID director, we were challenged with the emergence or reemergence of numerous infectious diseases with varying degrees of regional or global impact.
Included among these were the first known human cases of H5N1 and H7N9 influenza; the first pandemic of the 21st century (in 2009) caused by H1N1 influenza; multiple Ebola outbreaks; Zika in the Americas; SARS caused by a novel coronavirus; Middle East respiratory syndrome caused by another emergent coronavirus; and of course COVID-19, the loudest wake-up call in more than a century to our vulnerability to outbreaks of emerging infectious diseases.
One highly successful element of the response to the pandemic was the rapid development — enabled by years of investment in basic and applied research — of highly adaptable vaccine platforms such as mRNA (among others) and structural biology tools to design vaccine immunogens.
Over the years, many subspecialties of medicine have benefited dramatically from breathtaking technological advances.
The same can now be said of the field of infectious diseases, particularly with the tools we currently have for responding to emerging infectious diseases, such as the rapid and high-throughput sequencing of viral genomes; the development of rapid, precise multiplex diagnostics; and the use of structure-based immunogen design combined with novel platforms for vaccines.
If anyone had any doubt about the dynamic nature of infectious diseases and, by extension, the discipline of infectious diseases, our experience over the four decades since the recognition of AIDS should have completely dispelled such skepticism.
Today, there is no reason to believe that the threat of emerging infections will diminish since their underlying causes are present and most likely increasing.
The emergence of new infections and the reemergence of old ones are largely the result of human interactions with and encroachment on nature.
As human societies expand in a progressively interconnected world and the human-animal interface is perturbed, opportunities are created, often aided by climate changes, for unstable infectious agents to emerge, jump species, and in some cases, adapt to spread among humans.
An inevitable conclusion of my reflections on the evolution of the field of infectious diseases is that the pundits of years ago were incorrect and that the discipline is certainly not static; it is truly dynamic.
In addition to the obvious need to continue to improve our capabilities for dealing with established infectious diseases such as malaria and tuberculosis, among others.
It is now clear that emerging infectious diseases are truly a perpetual challenge.
As one of my favorite pundits, Yogi Berra, once said, "It ain't over till it's over."
Clearly, we can now extend that axiom: it's never over when it comes to emerging infectious diseases.
As infectious-disease specialists, we must be perpetually prepared and able to respond to the perpetual challenge, concluded Dr. Fauci's recent article.
PrecisionVaccinations publishes fact-checked, research-based vaccine news manually curated for mobile readers.
Our Trust Standards: Medical Advisory Committee