Taking Hepatitis A Off Restaurant Menus in 2019
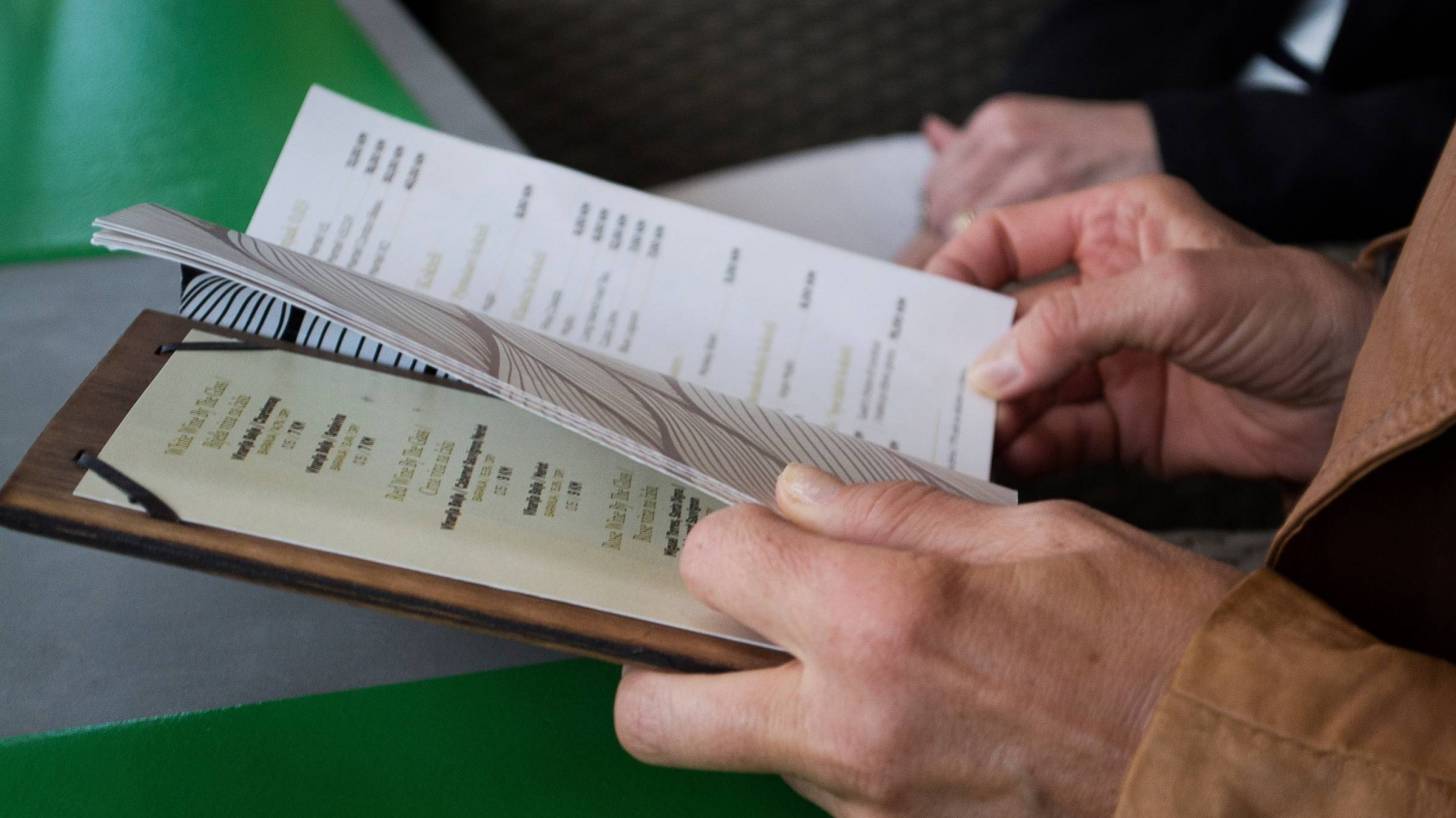
Besides worrying if your food or coffee is served hot during 2019, restaurant patrons may need to ask managers if their staff has been vaccinated against the hepatitis A virus.
This question is relevant since throughout 2018, and at the beginning of January 2019, many well-known restaurant chains reported hepatitis A alerts related to infected staff.
This partial list of restaurants reporting hepatitis A alerts include, but is not limited to, the following companies:
- Applebee’s
- Arby’s
- Bob Evan’s
- Buffalo Wild Wings
- Burger King
- Cheddars
- Dominos Pizza
- Frisch’s Big Boy
- IHOP
- Jimmy John’s
- Kroger
- Little Caesars Pizza
- McDonald's
- On The Border
- Outback Steakhouse
- Pizza Inn
- Pizza Hut
- Taco Bell
- White Castle
- Zaxby's
And these alerts led various states to report increased hepatitis A cases.
As an example, the state of Kentucky reported 3,265 residents have been impacted since 2017.
And, the state of North Carolina reported 56 confirmed cases, 42 hospitalizations and 1 death related to the 2018 hepatitis A outbreak.
According to the Centers for Disease Control and Prevention (CDC), as of December 15, 2018, there were 10,582 confirmed hepatitis A cases in the USA.
The 3 largest groups affected by the ongoing, multi-state, Hepatitis A virus outbreak are intravenous drug users, the homeless, and men who have participated in sexual intercourse with other men.
Additionally, food-service workers represent another sizable, at-risk population since their daily responsibilities include directly handling food and drink, said the CDC.
There is also an overlap between intravenous drug users and part-time food-service workers in some communities, says Dr. Sarah Moyer, Medical Director of Public Health and Wellness for the state of Kentucky.
“People who use drugs may seek part-time work at places like food-service establishments, leading to the potential for Hepatitis A spread...we encourage other businesses to either donate vaccine or immunize their employees against Hepatitis A,” Dr. Moyer said to Insider Louisville.
According to previous studies, the restaurant segment of the food-service industry has a long, sordid relationship with substance abuse and substance abuse disorders.
In 2015, a study conducted by The Substance Abuse and Mental Health Administration found the food services and hospitality industry to have the highest rates of substance use disorders of all employment sectors.
But, one national restaurant chain has just announced a significant effort that may reduce hepatitis A cases in its staff.
Starbucks is installing needle-disposal boxes in some bathrooms, as well as exploring other solutions to workers' concerns regarding improperly discarded syringes and the related health risks.
This decision was related to more than 3,700 people who signed a petition on Coworker.org, calling for Starbucks to place needle-disposal boxes in high-risk bathrooms.
Previously, in October 2018, Starbucks staff in Seattle reported to KIRO7 that they often encountered hypodermic needles on the job.
And, as a result of the hepatitis risk, they had to take antiviral medications to protect themselves from hepatitis.
The decision to install needle-disposal boxes in Starbucks locations could prompt industry-wide change, making restaurant workers' jobs safer amid the hepatitis A epidemic, reported Business Insider.
Foodborne hepatitis A outbreaks are relatively uncommon in the United States, says the CDC.
However, when outbreaks occur, intensive public health action may be required to contain them.
Food handlers play a critical role in preventing the spread of foodborne hepatitis. Although ready-to-eat foods can be contaminated when handled by a person who is shedding the virus.
As a general precaution for all communicable diseases, employees who handle food should be monitored for early signs of illness. Be observant when greeting employees and managers. Watch for symptoms such as coughing, sneezing and vomiting, and complaints of a sore throat, cramps or diarrhea.
Symptoms more specific to hepatitis include fever, fatigue, nausea and abdominal discomfort. These symptoms are sometimes followed by jaundice (yellowing of the eyes and skin). When these signs appear, an HAV diagnosis can be confirmed by a blood test.
By the time a person with HAV exhibits symptoms, they have already been shedding the virus in their stool for at least the previous two weeks. They may continue to pass the virus for another week after the symptoms have appeared.
Given the virus’s long incubation period, people who may have been exposed should be on the alert for early warning signs of the disease.
Burger King is another example of a national restaurant chain taking preventative action.
Burger King in Kentucky is now requiring hepatitis A vaccination for its employees, according to Kentucky Public Health Director Brent Blevins.
To prevent the spreading of hepatitis, the CDC says there are 2 brands of hepatitis A vaccines available, which are interchangeable.
Two monovalent hepatitis A vaccines, Vaqta and Havrix, are approved for people older than 1 year of age in a 2-dose series.
And, Twinrix is a combined hepatitis A and hepatitis B vaccine approved for people older than 18 years of age in the USA.
If you miss the 6-month timeline, you do not need to start the vaccination series over again, says the CDC. And, getting an extra dose of the hepatitis A vaccine is not harmful.
The CDC Vaccine Price List displays current hepatitis vaccine contract prices and general information.
And, hepatitis vaccine discounts can be found here.
Vaccines, like any medicine, can have side effects. You are encouraged to report negative side effects of vaccines to the FDA or CDC.
Our Trust Standards: Medical Advisory Committee