What Does the Next Pandemic Pathogen Look Like?

Preparing for future infectious disease outbreaks is a never-ending effort.
Historically, being prepared focused on the known list of pathogens derived from biological warfare agents and previous outbreaks.
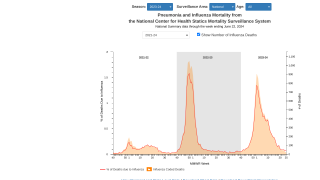
No exhaustive catalog of global catastrophic biological risk (GCBR) culprits exists, leaving the health community to rely on historical examples (e.g., 1918 Spanish Flu) to guide their preparedness priorities.
GCBRs are events in which biological agents could lead to a sudden, extraordinary, widespread disaster beyond the collective capability of national and international governments, and the private sector to control.
Which means, the current disease security protocol is obsolete.
To address this void, scholars from the Johns Hopkins Center for Health Security published a new report, “The Characteristics of Pandemic Pathogens.”
This report establishes a framework for identifying naturally occurring microorganisms that pose a global catastrophic biological risk and makes broad recommendations for improving GCBR preparedness efforts.
To formulate the findings and recommendations in their report, they reviewed published literature and reports on emerging infectious disease characteristics, the pathogenic potential of microbes, and other related topics; interviewed more than 120 technical experts from academia, industry, and government; and convened a meeting of a subset of those experts to discuss preliminary analysis of the information the team had gathered.
“Health security preparedness needs to be adaptable to new threats and not exclusively wedded to historical notions,” said Amesh Adalja, MD, project lead and senior scholar at the Center.
“A more active-minded approach to this problem will, in the end, help guard against a GCBR event occurring.”
The first and primary finding presented in the report outlines common characteristics of a potential GCBR-level pandemic pathogen.
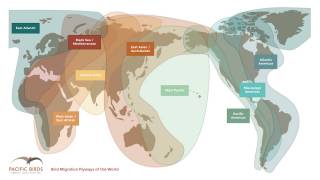
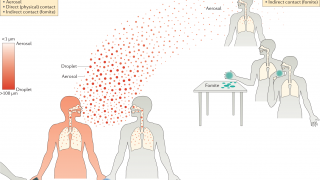
Its mode of transmission, the team concluded, will most likely be respiratory.
It will be contagious during the incubation period, prior to symptom development, or when infected individuals show only mild symptoms.
Finally, it will need specific host population factors (e.g., immunologically naïve persons) and additional intrinsic microbial pathogenicity characteristics (e.g., a low but significant case fatality rate) that together substantially increase disease spread and infection.
The report continues its findings with an explanation of the pandemic potential of certain categories of microbes, noting that RNA viruses are the biggest threat.
The project team’s preparedness-related findings are reflected in 8 key recommendations:
- Preparedness against GCBR-level threats should have a focused approach with some flexibility.
- Historical pathogen list-based approaches should not stand as permanent fixed ideas that stultify thinking on pandemic pathogens.
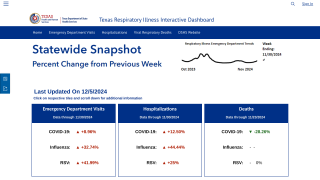
- Improving surveillance of human infections from respiratory-borne RNA viruses should become a higher priority.
- An increased emphasis on developing a specific pipeline of various antiviral agents for RNA respiratory viruses—both broad spectrum and virus-specific—would add resiliency against potential GCBR agents.
- Vaccines against RNA respiratory viruses—including a universal influenza vaccine—should be pursued with increased priority.
- A clinical research agenda for optimizing the treatment of respiratory-spread RNA viruses should be funded by pharmaceutical companies and medical device companies and pursued by clinical centers.
- A special review is warranted for respiratory-borne RNA virus research that could increase pandemic risks.
- Pursuing microbiologically specific diagnoses of infectious disease syndromes in all locations globally should become more routine.
“We hope policymakers and practitioners consider our recommendations in their work to strengthen health sector resilience and fortify pandemic preparedness,” said Adalja.
This project was supported by funding from the Open Philanthropy Project and is part of the Center’s extensive research and scholarship on GCBRs.
The Johns Hopkins Center for Health Security works to protect people from epidemics and disasters and build resilient communities through innovative scholarship, engagement, and research that strengthens the organizations, systems, policies, and programs essential to preventing and responding to public health crises. The Center is part of the Johns Hopkins Bloomberg School of Public Health and is located in Baltimore, MD.
Our Trust Standards: Medical Advisory Committee