HIV Vaccine Candidates Fail to Reduce Infections

The results of the PrEPVacc HIV vaccine trial conducted in Africa between 2020 and 2024 show conclusively that neither of the two experimental vaccine regimens tested reduced HIV infections among the study population.
The PrEPVacc vaccine trial results, announced at AIDS 2024 in Germany in July 2024, report more infections in the two vaccine arms than in the placebo arms. Still, the researchers say they cannot draw a definitive conclusion about this because the statistical ‘confidence intervals’ for the comparison are so wide, indicating high uncertainty.
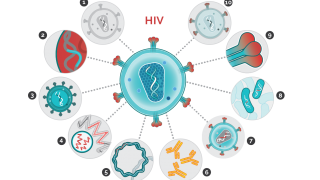
PrEPVacc tested two different combinations of HIV vaccines.
One regimen combined a DNA vaccine (DNA-HIV-PT123) with a protein vaccine (AIDSVAX B/E), and the other combined the same DNA vaccine, a modified non-dividing virus vector (MVA-CMDR), and a protein-based vaccine (CN54gp140).
The vaccination schedule included four vaccine injection visits: three over approximately six months and a fourth a year after enrolment.
The PrEPVacc trial was stopped in November 2023 when it became clear to independent experts monitoring the study data that there was little or no chance of the vaccines demonstrating efficacy in preventing HIV acquisition.
Dr Peter Gilbert, Principal Investigator, who is independent of the PrEPVacc study and has no ties with it, commented in a press release on July 23, 2024, “Given the PrEPVacc results that the estimated rates of HIV-1 acquisition were higher in the vaccine arms than the placebo arm, it is important to thoroughly quantify and communicate the precision available for drawing inferences about whether the vaccines truly elevated risk or, alternatively, a statistical fluke occurred and the vaccines were indeed safe."
"P-values are incomplete tools for this task because they cannot be interpreted in terms of the question, ‘What is the chance the vaccine elevated the acquisition rate?’
“To fill this gap, I conducted a Bayesian analysis that provides answers to this desired interpretation, using the same method that I previously applied to other HIV vaccine efficacy trials."
"The result was that, for each vaccine, there is close to a 50-50 chance that the vaccine elevated acquisition risk vs. the vaccine was safe, as a synthesis of results over multiple ways to do the analysis, most importantly considering different prior distributions for vaccine efficacy," added Dr. Gilbert.
As of August 2, 2024, the U.S. FDA has approved an HIV vaccine.
Our Trust Standards: Medical Advisory Committee