Will Gene Editing Cure HIV

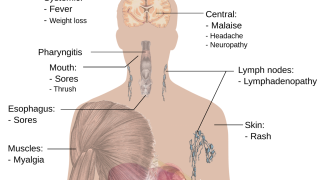
Recent announcements indicate innovative technologies may provide new clinical solutions for the 36.9 million people living with HIV/AIDS worldwide.
The current standard of care for these people of all ages is a combination of antiretroviral therapies, which may control the disease, but are not curative, as they cannot target integrated HIV-1 genomes, says HIV.gov.
Recently, a potential cure for human immunodeficiency virus type 1 (HIV-1) created with CRISPR-based editing of HIV proviral DNA was announced.
The participant was dosed in July 2022, with initial findings indicating EBT-101 has been well tolerated to date, announced San Francisco-based Excision BioTherapeutics, Inc.
"Dosing the first participant with EBT-101 is a landmark event that solidifies Excision's position as a pioneer in gene editing," said Daniel Dornbusch, Chief Executive Officer of Excision, in a related press release on October 15, 2022.
"It is the first time a CRISPR-based therapy targeting an infectious disease has been administered to a patient."
"In addition, it is expected to enable the first-ever clinical assessment of a multiplexed, in vivo gene editing approach."
EBT-101 is a unique, clinical-stage in vivo CRISPR-based therapeutic designed to cure HIV infections after a single intravenous infusion.
EBT-101 employs an adeno-associated virus (AAV) to deliver CRISPR-Cas9 and dual guide RNAs, enabling a multiplex editing approach simultaneously targeting three distinct sites within the HIV genome.
This allows for the excision of large portions of the HIV genome, thereby minimizing potential viral escape.
The participant continues to be monitored for safety and is expected to qualify for analytical treatment interruption (ATI) of their background antiretroviral therapy (ART) to evaluate a potential cure.
Rachel M. Presti, M.D., Ph.D., Associate Professor of Medicine at Washington University School of Medicine in St. Louis, MO, and Principal Investigator of the Phase 1/2 trial, added, "Using gene editing to target the HIV DNA reservoirs in human cells is a novel investigational approach, designed to cure HIV."
"We are well-positioned to collect key data in this first-in-human study to determine whether we can duplicate the success of this approach in animal models."
All participants in the study will be assessed for eligibility for an ATI of their background ART at Week 12.
Following the initial 48-week follow-up period, all participants will be enrolled in a long-term follow-up protocol.
For more information, see NCT05144386 (Phase 1/2 trial) and NCT05143307 (long-term follow-up protocol).
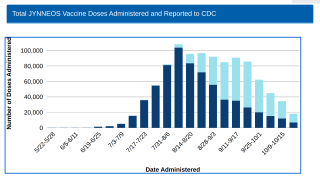
And on October 12, 2022, the journal International Journal of Infectious Diseases published a very positive systematic review and meta-analysis regarding COVID-19 vaccination and people living with HIV (PLWH).
Twenty-two studies with 6,522 subjects met the study's inclusion criteria.
This review concluded COVID-19 vaccines show favorable immunogenicity and efficacy in PLWH.
And a second vaccine dose is associated with consistently improved seroconversion, although it is slightly lower in PLWH compared with healthy individuals.
Additional strategies, such as a booster vaccination with mRNA COVID-19 vaccines, might improve seroprotection for these patients.
As of October 17, 2022, the U.S. FDA has not approved an HIV vaccine. Other breaking news is posted at PrecisionVaccinations.com/HIV.
PrecisionVaccinations publishes fact-checked, research-based vaccine news manually curated for mobile readership.
Our Trust Standards: Medical Advisory Committee