Pneumonia Diagnostic Discordance Occurred in 57% of Related Patients

Based on new research, pneumonia diagnoses at the hospital have been found to be less clear-cut.
More than half the time, a pneumonia diagnosis made in the hospital will change, either because someone initially diagnosed with pneumonia ended up with a different final diagnosis or because a final diagnosis of pneumonia was missed when a patient entered the hospital.
Discordances between initial and discharge occurred in 57% of related patients.
Among patients discharged with a pneumonia diagnosis and positive initial chest image, 33% lacked an initial diagnosis.
Among patients diagnosed initially, 36% lacked a discharge diagnosis, and 21% lacked positive initial chest imaging.
Published in the Annals of Internal Medicine on August 6, 2024, this study's results call into question much of the existing research on pneumonia treatment, which tends to assume that initial and discharge diagnoses will be the same.
These researchers say doctors and patients should consider this high level of uncertainty after an initial pneumonia diagnosis and be willing to adapt to new information throughout the treatment process.
Barbara Jones, MD, MSCI, pulmonary and critical care physician at the University of Utah Health and the first author of the study, found the results by searching medical records from more than 100 VA medical centers across the country, using artificial intelligence-based tools to identify mismatches between initial diagnoses and diagnoses upon discharge from the hospital.
More than ten percent of all such visits involved a pneumonia diagnosis, either when a patient entered the hospital when they left, or both.
“Pneumonia can seem like a clear-cut diagnosis,” Dr. Jones said in a press release, “but there is actually quite a bit of overlap with other diagnoses that can mimic pneumonia.”
Pneumonia is an infection in the lungs that typically stems from several kinds of germs, most often bacteria and viruses.
Furthermore, there are three types of pneumonia: Community-acquired, Healthcare-acquired, and Ventilator-associated.
The study also found that this uncertainty was often evident in doctors’ notes on patient visits; clinical notes on pneumonia diagnoses in the emergency department expressed uncertainty more than half the time (58%), and notes on diagnosis at discharge expressed uncertainty almost half the time (48%). Simultaneous treatments for multiple potential diagnoses were also common.
When the initial diagnosis was pneumonia, but the discharge diagnosis was different, patients tended to receive a greater number of treatments in the hospital.
Still, as a general rule, this study concluded these patients didn’t do worse than others.
However, patients who initially lacked a pneumonia diagnosis but ultimately ended up diagnosed with pneumonia had worse health outcomes than other patients.
“Both patients and clinicians need to pay attention to their recovery and question the diagnosis if they don’t get better with treatment.”
These findings highlight the need to recognize diagnostic uncertainty and treatment ambiguity in the practice of pneumonia-related care.
"The sum of these analyses suggests that initial pneumonia diagnosis is a complex process with substantial uncertainty that may previously have been underappreciated," the study authors wrote. These researchers say various immunizations can lower people's risk of pneumonia.
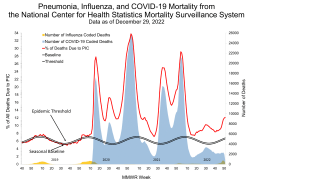
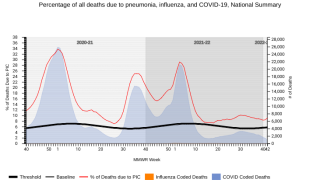
For example, annual flu shots have been found to reduce pneumonia cases.
As of August 2024, influenza vaccines became available at local pharmacies before the 2024-2025 flu season.
The primary Funding Source of this study was the Gordon and Betty Moore Foundation.
Our Trust Standards: Medical Advisory Committee