When Are Malaria Vaccines Most Effective

Malaria vaccine candidates have been in development since the 1960s, but innovative vaccines have made substantial progress in the last decade.
Gavi, the Vaccine Alliance, recently wrote that the recent launch of malaria vaccinations in Africa marks a turning point in the age-old battle against this mosquito-transmitted disease.
While both World Health Organization-recommended vaccines target the same protein on the surface of malaria parasites and are expected to reduce malaria cases and deaths, interpreting their efficacy can be challenging.
This is because efficacy measurements are not directly comparable due to differences in clinical study design.
Various studies have shown that vaccine efficacy is improved when using a seasonal approach, which means administering vaccines seasonally compared to an age-based approach.
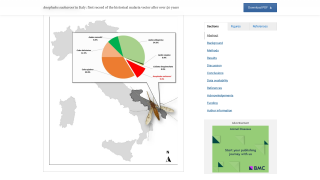
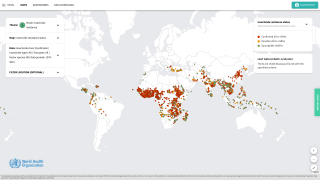
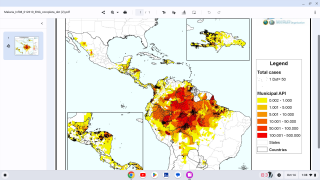
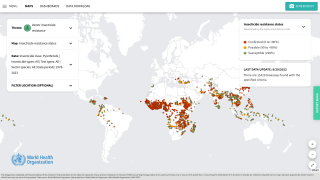
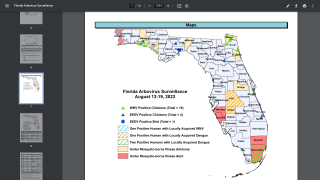
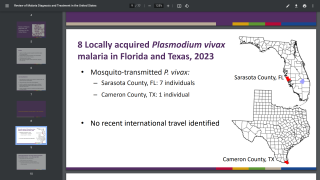
A recent study observed that rainfall and temperature are significant drivers of malaria seasonality in all parts of Sub‐Saharan Africa except in West Central Africa. In Sub‐Saharan Africa, seasonal malaria transmission is sustained at temperatures well above 15°C or below 40°C with maximum monthly rainfall not exceeding 600 mm.
For example, the phase 3 clinical trial of the R21/Matrix-M™ vaccine evaluated an age-based vaccination approach in three study sites and seasonal vaccination in two.
Age-based vaccination in the R21 trial included study sites in low—to moderate-transmission areas but did not include sites with year-round high transmission settings.
When the R21 vaccine was provided just before the malaria season in areas of seasonal transmission, malaria episodes were reduced by 75% in the first year following vaccination.
This is important because neither malaria vaccine provides complete protection against infection.
Both vaccines target malaria parasites during the ‘sporozoite’ stage of their lifecycle, where they first enter the human body and begin replicating in liver cells.
“In areas – and periods – with high transmission, the immune system is under a significant assault due to repeated biting from mosquitos,” says Dr. W. Scott Gordon, Head of Gavi’s Malaria Vaccine Programme, in a VaccinesWork article published on July 29, 2024.
“Each bite can transmit as many as 1,000 sporozoites, so even a tiny proportion of those getting through can result in the immunized child still coming down with malaria and lower measured efficacy from the vaccine.”
“This is one reason why WHO prioritizes the use of malaria vaccines in moderate to high transmission areas, where public health impact is expected to be highest.”
“We don’t know what the duration of protection with R21 is because it hasn’t been studied for long enough yet (as clinical trials are ongoing),” said Prof Brian Greenwood at the London School of Hygiene and Tropical Medicine, UK.
So, where does this leave us?
The bottom line is that two effective malaria vaccines are now available in Africa, ensuring millions of children have access to malaria prevention.
The completed, unedited article by Linda Geddes is posted at this link.
The University of Oxford Jenner Institute created R21 in 2017, and Novavax AB produces Matrix-M. As of August 2024, Mozambique, South Sudan, the Central African Republic, Côte d'Ivoire, Ghana, Nigeria, and Burkina Faso issued their authorization for deploying the R21 vaccine.
Our Trust Standards: Medical Advisory Committee