drMonoclonal Antibodies May Prevent Malaria

One dose of a new monoclonal antibody discovered and developed at the US National Institutes of Health (NIH) safely prevented malaria for up to nine months in people exposed to the malaria parasite.
This small clinical trial is the first to demonstrate that a monoclonal antibody can prevent malaria in people.
The trial was sponsored and conducted by scientists from the Vaccine Research Center (VRC) of the National Institute of Allergy and Infectious Diseases (NIAID), part of NIH, and was funded by NIAID.
NIAID Director Anthony S. Fauci, M.D., stated in a press release issued on August 11, 2021, “The results reported today suggest that a single infusion of a monoclonal antibody can protect people from malaria for at least nine months.”
“Additional research is needed, however, to confirm and extend this finding.”
The NIAID trial tested whether a neutralizing monoclonal antibody called CIS43LS could safely provide a high level of protection from malaria in adults following careful, voluntary, laboratory-based exposure to infected mosquitos in the United States.
CIS43LS was derived from a naturally occurring neutralizing antibody called CIS43.
Researchers led by Robert A. Seder, M.D., chief of the Cellular Immunology Section of the VRC Immunology Laboratory, isolated CIS43 from the blood of a volunteer who had received an investigational malaria vaccine.
The scientists found that CIS43 binds to a unique site on a parasite surface protein that facilitates malaria infection and is the same on all variants of P. falciparum sporozoites worldwide. The researchers subsequently modified this antibody to extend the time it would remain in the bloodstream, creating CIS43LS.
After animal studies of CIS43LS for malaria prevention yielded promising results, VRC investigators launched a Phase 1 clinical trial of the experimental antibody with 40 healthy adults ages 18 to 50 years who had never had malaria or been vaccinated for the disease.
The trial was led by Martin Gaudinski, M.D., medical director of the VRC Clinical Trials Program. It was conducted at the NIH Clinical Center in Bethesda, Maryland, and the Walter Reed Army Institute of Research (WRAIR) in Silver Spring, Maryland.
During the first half of the trial, the study team gave 21 participants one dose of CIS43LS by either an intravenous infusion or an injection under the skin. The infusions ranged from 5 to 40 milligrams per kilogram (mg/kg) of body weight, and the subcutaneous injections were 5 mg/kg.
Study investigators followed the participants for six months to learn whether the infusions and subcutaneous injections of the various doses of the experimental antibody were safe and well-tolerated. In addition, they measured the amount of CIS43LS in the blood to determine its durability over time.
In the second half of the trial, six participants who had received an intravenous infusion during the first half of the trial continued to participate. Four of these participants received a second antibody infusion, while the other two did not.
In addition, four new participants joined the study and received a single intravenous infusion of CIS43LS. Finally, another seven people entered the study as controls who did not receive the antibody.
All participants in the second half of the trial provided informed consent to be exposed to the malaria parasite in what is known as a controlled human malaria infection (CHMI).
In this procedure, volunteers are exposed to P. falciparum through bites of infected mosquitos in a carefully controlled setting, and they are closely monitored by medical staff for several weeks and promptly treated if they develop malaria.
CHMI has been used for decades to generate information about malaria vaccine candidates’ safety and protective effect and potential antimalarial drugs.
Nine participants who had received CIS43LS and six participants who served as controls voluntarily underwent CHMI and were closely monitored for 21 days. None of the nine participants who had received CIS43LS developed malaria within that period, but five of the six controls did.
The participants with malaria received standard therapy to eliminate the infection.
Among the nine participants who received CIS43LS and were protected, seven underwent CHMI approximately four weeks after their infusion. The other two participants had received their sole infusion during the first half of the study and were infected about nine months later.
These results indicate that just one dose of the experimental antibody can prevent malaria for 1 to 9 months after infusion.
Collectively, these data provide the first evidence that the administration of an anti-malaria monoclonal antibody is safe and can prevent malaria infection in humans.
To build on this finding, a more extensive Phase 2 clinical trial is underway in Mali to evaluate the safety and efficacy of CIS43LS at preventing malaria infection in adults during a six-month malaria season.
Peter D. Crompton is leading the trial, M.D., M.P.H., chief of the Malaria Infection Biology and Immunity Section in the NIAID Laboratory of Immunogenetics, and Kassoum Kayentao, M.D., M.P.H., Ph.D., a professor at the University of Sciences, Techniques and Technologies of Bamako, Mali. NIAID is sponsoring and funding the trial.
Study results are expected in early 2022.
In addition, VRC scientists are conducting further research on CIS43LS in the United States to determine the lowest dose that protects people from malaria infection.
“Monoclonal antibodies may represent a new approach for preventing malaria in travelers, military personnel, and health care workers traveling to malaria-endemic regions,” said Dr. Seder.
“Further research will determine whether monoclonal antibodies can also be used for the seasonal control of malaria in Africa and ultimately for malaria-elimination campaigns.”
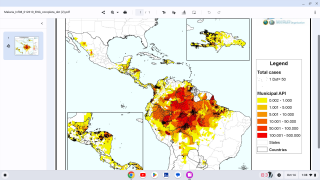
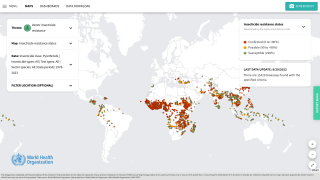
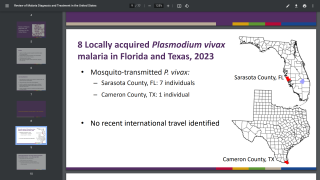
According to the World Health Organization, an estimated 229 million malaria cases occurred worldwide in 2019, resulting in an estimated 409,000 deaths, mostly in children in sub-Saharan Africa.
Malaria is caused by Plasmodium parasites, which are transmitted to people through the bite of an infected mosquito. The mosquito injects the parasites in a form called sporozoites into the skin and bloodstream. These travel to the liver, where they mature and multiply.
Then the mature parasite spreads throughout the body via the bloodstream to cause illness.
Thus, P. falciparum is the Plasmodium species most likely to result in severe malaria infections, which may lead to death if not promptly treated.
Laboratory and animal studies have demonstrated that antibodies can prevent malaria by neutralizing the sporozoites of P. falciparum in the skin and blood before they can infect liver cells.
The NIAID conducts and supports research at the NIH, throughout the United States, and worldwide—to study the causes of infectious and immune-mediated diseases and develop better means of preventing, diagnosing, and treating these illnesses.
The study’s findings were published in The New England Journal of Medicine.
Note: Mosquirix RTS,S/AS01e is the first vaccine that has demonstrated it can significantly reduce malaria, and life-threatening severe malaria, in young African children. In 2019, three African countries – Ghana, Kenya, and Malawi – are leading the vaccine’s introduction in selected areas of moderate-to-high malaria transmission as part of a large-scale pilot program coordinated by WHO.
Mosquirix does not provide complete protection against malaria caused by P. falciparum. The vaccine is designed to prevent the parasite from infecting the liver, mature, multiply, re-enter the bloodstream, and infect red blood cells, leading to disease symptoms.
PrecisionVaccinations publishes fact-checked research-based vaccine news.
Our Trust Standards: Medical Advisory Committee