Why Are Second Dengue Infections So Severe

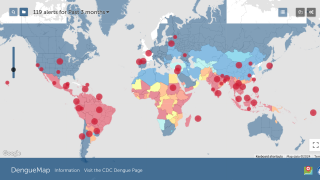
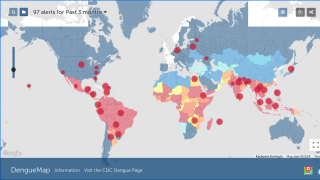
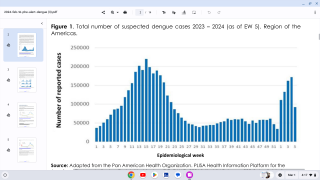
As the dengue virus continues to be a grade 3 global health concern in over 100 countries in 2024, an international research team led by Duke-NUS Medical School has identified a critical link between the body's initial immune response, its defense against reinfections and secondary infections, which become risk factors for developing severe disease.
On September 20, 2024, these researchers announced that they found that natural killer T (NKT) cells influence whether the response generates protective antibodies that neutralize the virus or harmful ones that could exacerbate the disease in future infections.
They reported that an initial infection with one of dengue's four serotypes does not provide immunity against the others. This means a different serotype can reinfect a person.
These observations illustrate how early innate immune responses during primary infections can influence secondary infection outcomes.
The researchers were intrigued by the fact that people infected with dengue have high concentrations of NKT cells in their skin, where the virus initially enters the body. Although many immune cells respond to the infection, NKT cells are among the first to act.
Integrating features of natural killer T cells, these unique immune cells link the innate and adaptive immune systems and play a key role in regulating immune responses.
When NKT cells are active during the initial dengue infection, they help establish a strong immune memory that protects against subsequent infections. In other words, NKT cells recruited to the skin at the start of an infection can influence immune responses for months or even years.
In addition to combating the virus directly in the skin, NKT cells also help to establish a supportive immune environment in nearby lymph nodes. This facilitates the production of effective antibodies, essential for neutralizing the virus and providing long-term protection by other immune cells.
"Our study shows that NKT cells not only shape the immune response to an initial dengue infection but also play a pivotal role in determining the severity of future infections," stated Associate Professor Ashley St John from the Program in Emerging Infectious Diseases at Duke-NUS, is senior author of the study published in the Journal of Clinical Investigation on August 1, 2024.
"Understanding this process is crucial, as it can lead to better strategies for protecting communities, especially in dengue-endemic regions, where severe reinfections can strain healthcare systems and impact public health," added St. John in a Duke-NUS press release.
The immune system relies on two primary types of immune responses—Th1, which focuses on destroying threats once they have infected cells, and Th2, which combats pathogens like bacteria, parasites, and toxins outside cells.
This makes Th1 responses particularly effective against viruses such as dengue. The researchers discovered that NKT cells drive dengue-specific Th1 responses, producing "good" antibodies that neutralize the virus.
In a pre-clinical model, the team found that the immune systems lacking functional NKT cells produce Th2-type antibodies, which are less effective against viruses. This leads to inadequate protection against reinfection with the same strain.
More importantly, it can also cause a phenomenon known as antibody-dependent enhancement, where "bad" antibodies from the initial infection exacerbate the disease during later infections with different strains.
This can make a secondary dengue infection more severe than the initial one.
Patients with primary dengue infections who developed Th1-associated antibodies linked to NKT cell activity had better outcomes. In contrast, those with secondary infections who produced high levels of Th2-associated antibodies were more likely to experience severe disease.
Co-senior author and Adjunct Senior Research Fellow at Duke-NUS, Dr. Abhay Rathore, who is also from the Department of Pathology at Duke University Medical Center, said, "Understanding how immune cells generate strong early responses can help us design vaccines that utilize NKT cells and Th1 responses for better antibody and memory cell production.
"This approach could enhance dengue vaccine effectiveness and safety, especially for those with prior exposure, and allow for personalized treatment by monitoring antibody levels to assess the risk of severe disease."
From a protection perspective, the United States is no longer offering dengue vaccines. The previously U.S. FDA-approved Dengvaxia was withdrawn from the market in early 2024
However, about 40 countries are in the process of offering Takeda's QDENGA® dengue vaccine, which the World Health Organization has recommended since 2023 and added to its List of Prequalified Vaccines in May 2024.
Our Trust Standards: Medical Advisory Committee