The Americas Set An Unfortunate Dengue Record

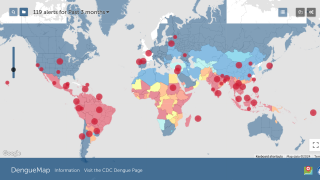
The Pan American Health Organization (PAHO) reported 2,733,635 confirmed Dengue Fever cases so far in 2019.
This is the largest number of Dengue cases recorded in the history of Dengue in the Americas and has already exceeded by 13 percent the total number of cases reported in 2015, the previous record year.
The PAHO Region of the Americas has also confirmed 1,206 Dengue-related fatalities, as of November 11, 2019.
The country with the highest incidence rate in the Americas is Brazil with 2,069,502 cases and 702 fatalities, as of Week #42 data.
Within the South American country of Brazil, the highest incidence rates are located in the states of Minas Gerais and São Paulo.
The next 4 highest-ranked countries in the Americas are located in the Central American Isthmus: Belize, El Salvador, Honduras, and Nicaragua.
In the USA, the US Centers for Disease Control (CDC) confirmed 865 travel-related Dengue cases in 2019 and issued a Level 1 Travel Alert on October 2, 2019, related to the Dengue outbreak in the Americas.
In the state of Florida, a 2nd Alert was issued by the Department of Health in October 2019.
As of November 9th, Florida DOH has confirmed 341 travel-associated cases and 12 locally-acquired dengue fever cases, primarily in Miami-Dade (10) County this year.
Dengue Clinical Overview
Dengue remains a public health problem in the Americas despite the efforts of the Member States to stop and mitigate the impact of epidemics. The infection can be asymptomatic or show with a broad clinical spectrum that includes serious and non-serious ways of expression.
After incubation, the disease begins abruptly and goes through three phases: The Febrile, Critical, and Recovery stages, says the PAHO.
1. Febrile Phase
- This acute febrile phase lasts 2-7 days and is usually accompanied by skin flushing, erythema, generalized body pain, myalgia, arthralgia, headache, and retro-orbital pain. Minor hemorrhagic manifestations, such as petechiae and ecchymoses in the skin may occur. Patients, who improve after the initial fever, are considered dengue without warning signs.
- Problems that may arise in the febrile phase: dehydration, high fever associated with neurological disorders, and seizures in young children.
2. Critical Phase
- After the fever abates, the patient may experience within the first 3-7 days of illness an increase of capillary permeability parallel with increased hematocrit levels. This marks the beginning of the critical phase with the highest risk of developing plasma leakage with or without hemorrhage, known as severe dengue. Patients who clinically worsen after the fever subsides should be monitored for warning signs and hemorrhagic manifestations.
- Problems that can occur in the critical phase: shock by plasma extravasation, severe bleeding, and serious organ impairment.
3. Recovery Phase
- Most patients survive the acute phase (which does not exceed 48 to 72 hours), with timely initiation of judicious fluid management and careful monitoring of the patient during the critical phase, and enter the recovery or convalescent phase. There is a general improvement in the patient: appetite recovers, gastrointestinal symptoms improve, hemodynamic status stabilizes and diuresis increases.
- Problems that can occur in the recovery phase are overload (if intravenous fluid therapy has been excessive or has been extended in this period).
Furthermore, the PAHO says Dengue needs to be addressed as a single disease with different clinical presentations ranging from benign conditions to severe clinical courses and outcomes that may lead to death.
There are 4 serotypes called DENV-1, DENV-2, DENV-3, and DENV-4. Previous research has shown infection with one serotype produces lifelong immunity against that serotype reinfection.
Successive infection with 2 different DENV serotypes is a risk factor for developing Severe Dengue, which has a greater fatality rate.
Dengue Transmission
The Aedes aegypti and Aedes albopictus mosquitoes are transmitters of dengue. The Aedes aegypti female mosquitos are the main source of dengue transmission. These species bite during the day, with the most active feeding period 2 hours before and after dawn and dusk.
In addition, new research indicates the Dengue virus can be transmitted during sex between humans.
The most recent detected case is a man who did not travel outside of Madrid, Spain. He developed symptoms mid-September 2019. This case is classified as autochthonous.
After confirmation of this case, his partner presented similar symptoms starting in September and was later tested and confirmed positive for dengue. This person had a recent travel history to Cuba and to the Dominican Republic, and this case was classified as imported.
Entomological investigations at the Madrid residence and surrounding area were negative, with no adult forms of Aedes albopictus detected.
And, genetic sequencing confirmed that the virus strain of both cases was identical. Further investigations showed that the virus is also similar to dengue viruses circulating in Cuba.
Dengue Prevention & Treatment
Treating Dengue patients can be expensive. According to the American Society of Tropical Medicine and Hygiene’s June 2019 report, the treatment costs to international travelers in out-of-pocket direct and indirect costs average $992 per episode.
According to the PAHO, there are personal prevention measures that are effective in preventing the transmission of the Dengue virus to healthy people, such as the following:
- Patients infected with the dengue virus are the reservoir of infection for other people both at home and in the community. Therefore, public health measures to minimize the exposure of patients to mosquitoes are critical in preventing the spread of the virus and, consequently, of the disease.
- Patients, other household members, and the affected community must be informed about the risk of transmission to others and ways to minimize this risk by reducing the vector population and human-vector contact.
- At home, use wire-mesh/mosquito nets on doors and windows.
- Patients should rest under mosquito nets, impregnated, or not, with insecticide.
- The patient, as well as other members of the household, must wear long sleeves (when ill persons are in the house) to cover extremities.
- Repellents containing DEET, IR3535, or Icaridine can be applied to exposed skin or clothing, and its use must be in strict accordance with the instructions on the product label.
Regarding preventive vaccines, Dengvaxia is the only approved dengue vaccine in the USA and about 20 other countries. Dengvaxia is indicated for the prevention of dengue disease caused by dengue virus serotypes.
The Dengue vaccine candidates in clinical studies include Takeda TAK-003, Merck V180, and Butantan Institute TV003/TV005.
The CDC says any vaccine can cause side effects, which should be reported to a healthcare provider ASAP.
Dengue News is published by Vax-Before-Travel.
Our Trust Standards: Medical Advisory Committee